- Pharmaceutical Technology-08-02-2005
- Volume 29
- Issue 8
Variable Air Velocity within Stability Chambers A Possible Cause of Out-of-Trend Stability Results
Stability data that do not follow the expected trend in comparison with other stability batches or previous results collected during a stability study are considered out-of-trend (OOT) results. OOT stability results recently have gained the attention of regulatory agencies and as a result, the approach for identifying and investigating OOT results has become a topic of increased discussion. One example is a 2003 article by the PhRMA Chemistry, Manufacturing, and Controls Statistics and Stability Expert Teams, which was intended to initiate dialogue on how to address OOT results (1).
Stability data that do not follow the expected trend in comparison with other stability batches or previous results collected during a stability study are considered out-of-trend (OOT) results. OOT stability results recently have gained the attention of regulatory agencies and as a result, the approach for identifying and investigating OOT results has become a topic of increased discussion. One example is a 2003 article by the PhRMA Chemistry, Manufacturing, and Controls Statistics and Stability Expert Teams, which was intended to initiate dialogue on how to address OOT results (1).
A critical aspect of handling OOT stability results is determining the reasons for their occurrence. If the causes are understood, OOT results can be prevented, thus saving manufacturers the hassles of their identification and investigation, including questioning by regulatory agencies.
In a previous article in this journal, the authors discussed various situations of equality or inequality in the slopes and intercepts of the stability data generated from studies conducted on three registration batches (2). A situation was examined in which the three batches could give the same intercept but different slopes. This difference in the rate of drug loss among the three batches was linked to storage factors. Accordingly, it was determined that how products are stored in a stability chamber also can cause OOT results during stability testing. In general, batches of products are stored in various locations in a chamber, depending upon the space available at the time. If the environmental conditions are not the same throughout a chamber, the stability test results of the stored batches may vary.
When stability test equipment is installed, the equipment manufacturer normally validates temperature and humidity control at the center of an empty chamber. Multipoint calibration is performed rarely, generally only when the drug manufacturer insists on it. In addition, operational qualification rarely is conducted in a chamber stacked with products. Accordingly, performance validation of stability chambers by drug manufacturers should include monitoring temperature and humidity at various locations in the chamber to ensure uniform environmental conditions. Unfortunately, this practice is not widely followed. Thus, batches placed in various locations in a stability chamber may be exposed to a variety of environments, which may cause OOT results.
Figure 1a: Internal design of the stability chamber used in the study. View shows the locations of the two fans.
Air velocity variations within a stability chamber also may contribute to OOT results. Air velocity normally is not considered when validation studies of stability chambers are conducted. For this reason, a study was conducted to examine the results of variable air velocity within a stability chamber. The study found that variable air velocity within a chamber led to variations in moisture gain by a hygroscopic drug. Therefore, hygroscopic drug products are expected to show variable stability patterns when stored under variable air-velocity conditions.
Experimental
Material. Ethambutol hydrochloride was obtained as a gift sample from Panacea Biotec Ltd. (Lalru, India).
Equipment. A stability chamber (Model KBWF720, WTB Binder, Tuttlingen, Germany) was maintained at 40 ±1 °C and 75 ±3% relative humidity (RH). A digital thermohygrometer (Cole-Parmer, Vernon Hills, IL) was used to record temperature and humidity values at various locations inside the chamber. Linear air velocity (ft/min) in the chamber was measured with an anemometer (AM-4201, Lutron, Taipei, Taiwan) consisting of a vane probe with fan and a display unit. Weights were measured on a precision balance (AG135, Mettler Toledo, Greifensee, Switzerland).
Figure 1b: Internal design of the stability chamber used in the study. View shows air-entry points and shelf slots.
Interior layout of the chamber. The stability chamber's interior design is shown in Figure 1. Figure 1a shows a front view of the chamber, highlighting the presence of two fans on the rear wall. Figure 1b shows air-entry slits and slots for the shelves on the interior side wall of the chamber. Air-entry points also were present on the right side of the chamber. In total, there were 15 shelf slots. Air-entry points were present at shelf slots 2–7 and 9–12 and absent from shelf slots 1, 8, and 13–15.
Mapping the chamber to record humidity, temperature, and air velocity. To map the chamber for temperature, humidity, and air velocity measurements at various locations, all shelves were removed except one. This shelf was marked with 23 test locations (see Figure 2). The shelf was placed initially on the upper-most slot (slot 1) and then shifted, level by level, to the lower slots. Temperature, humidity, and air velocity were recorded at all 23 points when the shelf was placed at each level. Air velocity was measured twice at each location, once with the vane probe in a horizontal position and then again with the vane probe upright, to identify even minute amounts of circulating air at each location. The chamber was allowed to equilibrate for ~2 h before measurements were recorded after the shelf was moved to the next slot.
Figure 2: Diagram of a shelf marked with the locations where temperature, humidity, and air velocity were recorded. Drug samples were placed at these locations to determine the rate of moisture gain by ethambutol hydrochloride.
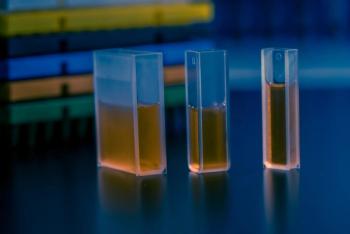
Moisture-gain studies. Moisture-gain studies were carried out using ethambutol hydrochloride, a hygroscopic substance. The drug was dried at 30 °C under 630 mm Hg pressure for ~7 h. The dried drug was gently ground with a mortar and pestle to remove all lumps and stored in an airtight container in a desiccator. Next, 300 mg of drug were dispensed into a 10-mL open glass beaker and transferred immediately to the stability chamber. The beaker was withdrawn periodically for weighing and then immediately returned to the chamber. The studies were conducted for 32 h.
Results and discussion
Control of temperature and humidity. Temperature and humidity values were within ±1 °C and ±3% RH, respectively, at all locations and at all shelf slots. These results indicate that the chamber maintained strict control of temperature and humidity throughout, thus conforming to current regulatory requirements (3).
Air velocity. In contrast, air velocity varied not only from one location to another on a single shelf, but also among slots (see Table I). Air velocity was the fastest near the two fans (at locations L1 and R1 on shelf 8), followed by the points near the air-entry points on both the sides of the chamber (at locations L9 and R9). Air velocity was lower at other locations on the same shelf, with the lowest velocity at locations L3, L7, L10, R3, R7, and R10, which were in the middle of the shelf, furthest from the air-entry locations on the sides of the chamber.
Table I: Air velocity (ft/min) measured at various locations in a stability chamber.*
Maximum air velocity was observed at the centermost shelf slots (slots 7–9), and was the lowest at the upper and lower slots. The upper slots, however, showed faster air velocity than the lower slots because of the tendency for hot air to rise.
Moisture-gain studies. Moisture gain was studied initially only at the top , middle, and bottom shelf slots (1, 8, and 15, respectively). The beakers were kept at a single point in each case. Moisture-gain curves to 8 h are shown in Figure 3. The rate and extent of moisture gain varied among the three shelf slots, with the highest moisture gain occurring on the middle shelf and the lowest on the bottom shelf, which corresponded to the variation in air velocity listed in Table I. This result appears to indicate that air velocity had a strong influence on the amount of moisture gain by the hygroscopic drug.
Figure 3: Moisture gain by ethambutol hydrochloride when stored in an open beaker at the top, middle, and bottom shelf slots. The beaker was placed at the same location on the shelf each time. The weight gain was monitored for 8 h.
A study was carried out to correlate moisture gain rates to air velocity. For this test, shelf slot 8 was selected because maximum air velocity and moisture gain were observed on that shelf slot. Open beakers containing ethambutol hydrochloride were kept at new locations showing air velocities of 0, 50, 100, 200, and 300 ft/min, and the moisture gain over time was measured. Studies were carried out in triplicate. Moisture-gain curves and a plot of air velocity versus the rate of moisture gain (slope of linear plots up to 8 h) are are shown in Figures 4a and 4b, respectively. Figure 4b clearly shows a linear trend among the points, thus confirming that moisture gain was directly related to air velocity.
Figure 4: The influence of air velocity on moisture gain by ethambutol hydrochloride. Figure 4a shows the moisture-gain profiles, and Figure 4b shows a plot of the rate of moisture-gain versus air velocity.
Later, more-intensive studies were performed by measuring the moisture gain by ethambutol hydrochloride at all 23 locations on a single shelf, and then repeating the study at several shelf slots (slots 1, 3, 5, 7–9, 12–13, and 15). The moisture gain at 8 h varied greatly from one location to another (see Figure 5). As expected, the locations near the air-entry points (locations L9 and R9) and the air exit points (locations L1 and R1 on shelf slot 8) showed the highest rate of moisture gain because the air velocities at those locations were faster than the air velocities at other locations on the same shelf. Samples placed at locations L1 and R1 at shelf slot 8 almost liquefied within 8 h. Another extreme situation occurred at locations L10 and R10, where the anemometer was unable to record air flow at almost any shelf slot. The samples at these locations could not reach a plateau of moisture gain even after 32 h. The center locations (C1–C3, see Figure 2) showed average moisture gain, except location C3, where greater fluctuation was observed. This point was located at the joint of the two glass panes of the inner door. The results at locations L5 and R5 were somewhat similar to C3. Overall, the rate of moisture gain was higher on the left side of the chamber than on the right. This result corresponded to the air velocity values, which were higher on the left side (see Table I).
Figure 5: Moisture gain by ethambutol hydrochloride after 8 h at each of the 23 locations on a shelf placed on shelf slots 1, 3, 5, 7, 8, 9, 12, and 15.
The same variations in moisture gain at 8 h were observed when the studies were repeated at other shelf slots (see Figures 6 and 7). Similar to the results observed during the initial studies, the highest rate of moisture gain was on the middle shelf slots (7, 8, and 9), followed by the upper shelf slots (1 and 3) and the bottom slots (13 and 15). In addition, the moisture gain at 8 h at location 7 was exactly the same on the left and right sides of every shelf. Because this location was located halfway between the rear wall and the chamber door, it was the least affected by air-turbulence caused by fans or air-entry points. Figure 7 confirms that moisture gain was similar at central locations C1 and C2, but was different at location C3, near the joint between the glass doors.
Figure 6: Moisture gain by ethambutol hydrochloride after 8 h at shelf locations L1âL10 and R1âR10. The study was conducted at shelf slots 1, 3, 5, 7, 8, 9, 12, 13, and 15.
The reason moisture gain depended on air velocity. The relationship of moisture gain to air velocity can be attributed to the fact that a faster rate of air flow above an open beaker quickly replenishes hot and humid air in that area and allows the hygroscopic drug to absorb moisture at a faster rate. In the study, the rate of moisture gain decreased when air velocity fell (see Figure 4b). In general, the maximum difference in moisture gain was observed at the 8-h point, but the total moisture gain at the plateau was the same for the drug stored at all locations (see Figure 4a). This result indicates that only the rate of moisture gain was influenced by air velocity and not the equilibrium moisture gain.
Figure 7: Moisture gain by ethambutol hydrochloride after 8 h, after storage at three central locations (C1â3) on 15 different shelf slots.
The relevance of the findings with respect to OOT stability results. Products containing hygroscopic drugs usually are packed in barrier packaging to avoid moisture gain. But in some situations, manufacturers may take the risk of marketing products in packaging without a moisture barrier to reduce costs. Such packaging was observed in a study carried out on marketed antituberculosis fixed-dose combination products containing ethambutol hydrochloride, a highly hygroscopic drug (4). In that study, several products were marketed in simple poly(vinyl chloride) blisters. Those products gained significant amounts of moisture within the package when stored under accelerated conditions of temperature and humidity (40 °C and 75% RH). The presence of moisture resulted in extensive physical and chemical instability (5). In one case, a strip-packaged product containing isoniazid and ethambutol gained moisture through pinholes in the packaging material (4). This product was physically unstable and a fine sheet of powder was spread inside each of the tablet pockets, even in freshly purchased product (6). Hence, it is reasonable to link moisture gain by hygroscopic drugs to the stability of the product(s) containing them. In that respect, it is not out of place to expect that storing products containing hygroscopic and moisture-sensitive drugs in a stability chamber with variable air velocity can be responsible for variable rates of product decay and hence OOT results.
Conclusions
This study shows that pockets of varying air velocity can exist in a stability chamber, even under nearly homogenous temperature and humidity conditions. This study also demonstrates that in cases in which the stability of a drug is directly linked to moisture (i.e., finished pharmaceutical products containing hygroscopic and moisture-sensitive drug substances or excipients) a drug product's stability may be affected by its storage location within a stability chamber. Thus, storing batches of hygroscopic drug substances or their products in a stability chamber that has variable air velocity within the chamber can lead to out-of-trend stability results.
Considering that stability chambers generally are stacked during routine stability studies, the overall air-velocity conditions during routine use may be different from the conditions observed in the relatively empty chamber studied. The airflow pattern may change with the extent of chamber loading, the orientation of the samples placed in the chamber, and even with each withdrawal or loading of stability samples. In addition, the effect of air velocity in small chambers is likely to be different than in walk-in chambers, because of differences in size and the availability of empty space for air circulation. For these reasons, more-extensive studies should be carried out to examine moisture gain versus air velocity in small chambers as well as walk-ins, using various stacking and orientation arrangements for the same load level. Such additional studies may be necessary to correlate the observations of this study with real situations, and to further confirm that OOT results appear because of differences in airflow conditions at various storage locations, either within a chamber or from one chamber to another.
In addition, manufacturers of stability test equipment should seek innovative solutions to maintain uniform airflow even under fluctuating stacking conditions. Possible solutions include building a chamber with laminar air flow and removing sharp corners within the chambers. Also, the current method of installing exhaust fans directly in the sample storage area (see Figure 1) may require reconsideration. In the meantime, users may find it helpful to monitor air velocity as part of chamber qualification protocols. Implementing these propositions would demand extra work, but their implementation may reduce the occurrence of OOT results and even improve the general standards of pharmaceutical stability testing.
Ashwani Gaur is a postgraduate student, T.T. Mariappan and Hemant Bhutani are doctoral students, and Saranjit Singh, PhD,* is a professor and head of the department of pharmaceutical analysis at the National Institute of Pharmaceutical Education and Research, Sector 67, S.A.S. Nagar 160 062, India, tel. 191 172 2214682, fax 191 172 2214692,
*To whom all correspondence should be addressed.
References
1. PhRMA CMC Statistics and Stability Experts Team, "Identification of Out-of-Trend Stability Results, A Review of the Potential Regulatory Issue and Various Approaches," Pharm. Technol. 27 (4), 38–52 (2003).
2. S. Singh, "Stability Testing and Shelf-Life Determination According to International Guidelines," Pharm. Technol. 23 (6), 68–88 (1999).
3. ICH, "Stability Testing of New Drug Substances and Products" (International Conference on Harmonization, IFPMA, Geneva, Switzerland, 2002).
4. H. Bhutani, T.T. Mariappan, and S. Singh, "Behavior of Uptake of Moisture under Accelerated Conditions of Temperature and Humidity in the Absence and the Presence of Light, Part II: Packaged and Unpackaged Antituberculosis Products," Pharm. Technol. 27 (6), 44–52 (2003).
5. H. Bhutani, T.T. Mariappan, and S. Singh, "The Physical and Chemical Stability of Marketed Anti-Tubercular Fixed Dose Combination (FDC) Products under Accelerated Climactic Conditions," Int. J. Tuber. Lung Dis. 8 (9), 1073–1080 (2004).
6. H. Bhutani, T.T. Mariappan, and S. Singh, "An Explanation for the Physical Instability of a Marketed Fixed Dose Combination (FDC) Formulation Containing Isoniazid and Ethambutol and Proposed Solutions," Drug Dev. Ind. Pharm. 30 (6), 667–672 (2004).
Articles in this issue
over 20 years ago
August 2005over 20 years ago
I Only Am Escaped Alone to Tell Theeover 20 years ago
Riding the Waveover 20 years ago
In the Spotlight: Pharmaceutical Science & Technology Innovationsover 20 years ago
Manufacturers Face New Challenges Battling Global Threatsover 20 years ago
But They're Not Touching the Floor...over 20 years ago
The End of Process Validation As We Know It?over 20 years ago
Identifying MarksNewsletter
Get the essential updates shaping the future of pharma manufacturing and compliance—subscribe today to Pharmaceutical Technology and never miss a breakthrough.