- Pharmaceutical Technology-03-02-2019
- Volume 43
- Issue 3
Handle with Care
Bio/pharma companies facing new challenges in light of the increasing HPAPI market may benefit from outsourcing.
Editor's Note: This article was published in Pharmaceutical Technology Europe's March 2019 print issue.
Market growth in the high potency active pharmaceutical ingredient (HPAPI) sector is projected to be in the region of 8.5% of compound annual growth rate within the forecast period of 2018–2024, according to market research (1). This robust level of growth is driving a need for improvements in industry and particularly manufacturing standards due to the toxic nature of the molecules in development.
“The scope and scale of HPAPIs within the pharmaceutical industry is growing, with over 1000 smallâmolecule HPAPIs currently in development,” confirms Maurits Janssen, head of commercial development, API Development & Manufacturing, Lonza Pharma & Biotech. “Much of this increased focus originates from the potential of HPAPI ingredients to improve treatments for cancer and an increasing number of specialty companies focusing in this area.”
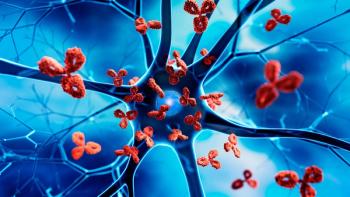
Additionally, there has been progressive interest in precision and personalized medicines, such as antibody-drug conjugates (ADCs), giving rise to more demand for highly toxic small molecules. ADCs are of particular relevance in light of more patient-centric approaches that are currently being favoured, thanks to their potential to reduce negative side effects of non-targeted oncology therapies due to their aimed action.
“Growth drivers for HPAPI medicines also include therapy areas beyond oncology,” specifies Janssen. “For example, antidiabetics and autoimmune diseases both account for 20% of the current production of smallâmolecule HPAPIs. While oncology therapies are becoming increasingly targeted and effective, thereby requiring smaller volumes of drug substance, other therapy areas have much larger patient groups and result in overall increased demand for HPAPI.”
Potent challenges
As is the case with many new candidate molecules, HPAPIs are frequently poorly soluble or feature bioavailability challenges, Janssen notes. As a result, HPAPIs require specialized enabling technologies to improve oral absorption and effective drug formulations, such as micronization, nano-milling, solid amorphous dispersions, and lipid-based approaches.
“Another challenge is the need for specialized procedures and know-how in terms of handling and containment of the drug substance, intermediates resulting from particle engineering and the manufacture of the finished drug product,” Janssen continues. “Given the increasing potency of these molecules, even small amounts of exposure can be harmful to workers.”
Further issues can arise when considering the therapeutic indication and resultant volume of product that needs to be handled. For some therapies, larger product volumes are required, which in turn need alternative containment solutions. According to Janssen, an effective containment procedure will include a high-standard containment strategy, a clear and standardized process for equipment start-up, a well-mapped-out cleaning procedure, and proven decontamination procedures. In addition, well-trained operators for running the equipment are key.
“Phase-appropriate processing to support feasibility assessments, clinical scale manufacture, and commercial production must be accessible for successful drug development using HPAPI molecules,” he adds. “Additionally, sterile fill/finish capabilities or specialized liquid-filled drug product technologies for safe HPAPI handling and consistent dosing are typically required.”
Yet, Janssen iterates that many bio/pharma companies lack the infrastructure, expertise, and capabilities associated with the specialized technologies required to handle HPAPIs. Therefore, an outsourcing partner with specialized development and manufacturing capabilities can offer benefits.
“Beyond training and processes, companies must also build the right culture-one that values a commitment to safety, quality, and performance,” he stresses. “After all, even with the right equipment in place, at least half of performance comes down to the well-trained people using it effectively.”
Benefits of outsourcing
Working with an external development and manufacturing partner that can help to manage highly potent compounds can not only help companies access specific technologies but can also potentially assist timeline management. “Working with a flexible partner with the appropriate capabilities can reduce costly delays-for example, in the scale-up and tech transfer process-and ensure that development schedules are kept,” says Janssen.
He further explains that by partnering with the right organization, companies can benefit from tailored options, fluidity, speed, and support in the HPAPI research, development and manufacturing process. “Ideally, such offers range from development of the active ingredient (API) to the final drug product formulation, integrating best practices from early clinical to commercial stages,” he adds.
In terms of containment, Janssen notes that a robust process that can support the correct use of highly potent compounds is the best solution. “An optimal containment strategy is twofold: a primary strategy that pertains to the reactor, filter, dryer, and their immediate usage; and a secondary strategy that describes additional containment for unit operations, requiring opening of the primary containment, for example maintenance,” he says. “In addition, well-defined and proven cleaning procedures also require consistent attention and caution from operators and these procedures need to be verified on a regular basis.”
When deciding upon a partner for containment solutions, Janssen explains that it is important the organization has substantial and proven experience with different types of containment solutions. Through this experience, the outsourcing partner should be capable of operating the entire HPAPI programme as efficiently as possible, while also ensuring product quality and operator health, he notes.
Regulatory harmonization: A work in progress
In Europe, the European Union’s good manufacturing practice guideline (EU GMP) sets out the minimum standard that needs to be met by drug manufacturers during production of medicinal products (2). The EU GMP guidance document is also supplemented by several annexes that specifically relate to product type or particular topics.
Only governmental authorities are entitled to perform GMP inspections, and each European member state executes its own inspections. “Europe is working to ‘harmonize’ legislation regarding manufacturing, containment and handling for toxic substances and thus the differences between the European member states may be reduced in the future,” suggests Janssen.
Current political changes are set to disrupt the region’s standardization, however. “Of course, Brexit stands to remove the United Kingdom from the European harmonization, with the relocation of the European Medicines Agency already underway,” Janssen continues. “But, Brexit’s impact on the European pharmaceutical industry remains unclear.”
Simultaneously, Switzerland is in discussions with the EU concerning legislative harmonization, but Janssen reveals that in general Switzerland and the EU are already quite aligned. “For handling of highly potent compounds, most of the relevant Swiss legislation is around safety, health and environment, and these are already rather well defined,” he says. “New regulations may influence transportation of these compounds.”
To further harmonize the GMP inspections with the United States, there is an important mutual reliance initiative ongoing between the European Medicines Agency (EMA) and the US Food and Drug Administration (FDA) with the goal to increase exchange of information on GMP inspections (3,4). On a global scale, there has been a gradual coming together of Europe and the US through a Mutual Recognition Agreement (MRA) that enables inspection standards to be deemed as equivalent between the two regions. Additionally, the MRA between the EU and Japan, operational since 2004, was extended in 2018 to include sterile medicines, certain biological medicines, and APIs of any medicine covered in the agreement (5). An important contributor of the GMP harmonization that positively influences global GMP manufacturing requirements are efforts of the Pharmaceutical Inspection Convention and Pharmaceutical Inspection Co-operation Scheme (PIC/S), which now includes 52 state members (6).
“Overall, we see the regulatory landscape gradually harmonizing around the world as more of the world’s population gains access to effective medicines,” adds Janssen. “We view streamlined global regulations as a positive for our customers, as it means we can implement more common practices between countries where we operate.”
Conclusion
“As the HPAPI landscape continues to grow and change, pharma and biotech companies may find themselves facing new challenges in terms of manufacturing, handling and containment of highly potent compounds,” notes Janssen.
Yet, he specifies that the current and future challenges will extend beyond HPAPI, to include specialized processing and finished dosage forms. Additionally, challenges will be compounded as a result of the trend towards more specialized and patient-centric treatments.
“Companies developing innovative pharmaceutical products will likely benefit from external partnerships with organizations that have the technologies, expertise, and flexible capabilities that can help meet target product profiles and commercial objectives for HPAPI and the specialized drug products that use these compounds,” he concludes.
References
1. Market Research Engine, “High Potency API /HPAPI Market By Type of Manufacturer Analysis (Captive Manufacturers, Merchant Manufacturers); By Type of Synthesis Analysis (Synthetic HPAPIs Market, Biotech HPAPIs Market); By Type Analysis (Innovative HPAPIs, Generic HPAPIs) By Therapeutic Application Analysis (Oncology, Hormonal Disorders, Glaucoma) and By Regional Analysis-Global Forecast by 2018-2024,” marketresearchengine.com (April 2017).
2. EMA, “
3. EMA, “
4. FDA, “
5. PIC/S, “
6. PharmTech, “EU and Japan Strengthen Collaboration on GMP Inspection,” PharmTech.com, 18 July 2018.
Article Details
Pharmaceutical Technology Europe
Vol. 31, No. 3
March 2019
Pages: 18–19, 22
Citation
When referring to this article, please cite it as F. Thomas, “Handle with Care," Pharmaceutical Technology Europe 31 (3) 2019.
Articles in this issue
almost 7 years ago
Tablet Press Refurbishment: Why and How?almost 7 years ago
Embracing the Digital Factory for Bio/Pharma Manufacturingalmost 7 years ago
Caught in a Conundrumalmost 7 years ago
Strategic Screening for Solubility Solutionsalmost 7 years ago
Monoplant: Advantages of a Dedicated Facilityalmost 7 years ago
Rising to the Challenge of Biologic Drug Formulationalmost 7 years ago
Can the Price Ever be Right?almost 7 years ago
Europe Pushes for Global Easing of Generics Approvalsalmost 7 years ago
Key Considerations in Stability TestingNewsletter
Get the essential updates shaping the future of pharma manufacturing and compliance—subscribe today to Pharmaceutical Technology and never miss a breakthrough.