- Pharmaceutical Technology-03-02-2009
- Volume 33
- Issue 3
Extending Calibrations for Near Infrared Assay of Tablets Using Synthetic Modeling and Variance from Placebos
The authors extend the range of a near-infrared calibration model for tablet assay using production 'seed' spectra and synthetic spectra generated from placebos and 'pure' active pharmaceutical ingredient spectra.
The US Food and Drug Administration initiative for process analytical technology (PAT) has created interest in measuring pharmaceutical products upstream during processing for better quality and process control (1). Near infrared (NIR) spectroscopy has been a major analytical tool designated for PAT analysis because it is fast, accurate, nondestructive and requires no sample preparation. At-line solid dosage form analysis has become important for tablet assay and content uniformity because pharmaceutical manufacturers would like to measure more frequently than the 10 tablets per batch specified by US Pharmacopeia General Chapter ‹905› on content uniformity.
Laboratory methods for tablet assay and content uniformity are routinely performed with high-performance liquid chromatography (HPLC) and are usually time-consuming because they require lengthy calibration runs, the mixing of buffers, and the procurement and disposal of hazardous solvents. The analysis of 10 tablets for content uniformity could take hours and the results may not be available to the tablet press operators or for batch release for many days or even weeks after the tablets are compressed.
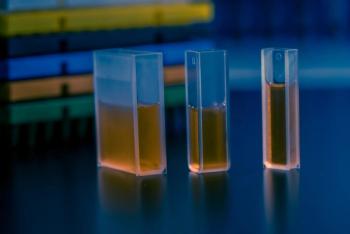
Figure 1 (ALL FIGURES ARE COURTESY OF THE AUTHORS.)
NIR spectroscopic analysis is an empirically based technique that requires the prediction method developer to analyze a calibration set of samples that represent the natural variation in the solid dosage form (2). It is often difficult to obtain the proper range of samples that would include slightly more than ±15% of the label claim. The process produces tablets normally distributed around the label claim, and the model developer cannot obtain tablets that are more than a few percent away from the nominal value. Therefore, to empirically develop a prediction model that can predict samples that may be ±15% of the label claim without extrapolation, synthetic methods are investigated.
Figure 2
This article discusses a method of obtaining a prediction method that uses only placebo tablets and samples containing an active pharmaceutical ingredient (API) from the product line. The natural variation range in the product line is extended with synthetic samples created by adding varying amounts of the pure-active spectrum to the placebos. Purely synthetic spectra lack the scattering variance of real tablets and would not create a robust prediction model. The placebos, which are often available from clinical studies, provide the real scattering and spectral variance seen in a calibration set.
Figure 3
Experiment
For this study, the authors used the XDS MasterLab NIR instrument (FOSS NIRSystems, Laurel, MD). The system can automatically measure multiple tablets after they are positioned in a special tray (see Figure 1). Spectra were collected in the transmission mode from 800 to 1650 nm with 0.5 nm data intervals and 32 scans were co-added to produce a single spectrum.
Figure 4
Ten chlorpheniramine maleate (CPM) tablets of nominal 1.0 mg and 10 placebo tablets of the same excipient composition were scanned on the MasterLab transmission instrument. The tablets from a 1.0-mg CPM batch were sent for HPLC analysis after NIR scanning. The spectra of the first five of the 1.0 mg tablets were averaged, and the placebo spectra were averaged. The other five tablets measured were saved for a validation set. The average placebo spectrum was subtracted from spectrum of the average of the five 1.0-mg tablets in the FOSS Vision software. This resulted in a simulated transmission spectrum of pure CPM. This spectrum could not be obtained in transmission because the pure CPM would have had to be pressed as a tablet.
Figure 5
The pure CPM spectrum was multiplied by factors to obtain a range of pure spectra from 85% to 115% in 5% increments of label claim. The average HPLC value for the five real tablet spectra was calculated. The average value was multiplied times each fraction from 0.85 to 1.15 to correct for the HPLC versus nominal tablet CPM values. The fractional pure spectra from 85% to 115% were then added to the 10 individual placebo spectra resulting in 70 spectra. The five real tablet spectra were added to the synthetic calibration set as "seed" spectra resulting in 75 spectra in the total calibration set.
Table I: Real tablet high performance liquid chromatography (HPLC) analysis and fraction adjusted by mean tablet value.
Discussion
Figure 2 shows the 75 raw NIR spectra from the calibration set. Figure 3 shows the spectrum of the simulated pure CPM. By taking the second derivative of the spectra, as shown in Figure 4, the baseline was normalized and the spectral features were enhanced so that the fanning out of the analytical region for CPM was observed at 1138 nm. The second derivative causes the absorption bands to be inverted and increase in the downward direction. The second derivative pretreatment was applied using a smoothing with a segment of 10 and a gap of 0. The standard normal variate (SNV) pretreatment was applied to reduce scattering effects. An integral thickness correction was applied as a math pretreatment to correct for tablet thickness and density variance from 1280 nm to 1350 nm.
Figure 6
Figure 5 shows the expanded second derivative of the aromatic CH stretch analytical band demonstrating the fanning out from 0.85 mg to 1.15 mg CPM (adjusted to 0.875 mg to 1.1838 mg from HPLC analysis). Table I shows real tablet values and the fractional adjustment that was made using the mean tablet value. The adjusted values are the constituent values that were used for modeling.
Figure 7
Partial least squares (PLS) regression was used to develop the prediction model. PLS uses principal component analysis and is a variation of principle component regression (PCR). The correct number of principal components or factors determination is aided by the Vision software supplied with the instrument by calculating where the predicted residual error sum of squares (PRESS) reaches a minimum (3). Although the PRESS does not reach a minimum until 13 factors, 6 were chosen as optimal allowing more than 10 calibration samples for each factor and considering possible degrees of freedom.
Figure 8
Figure 6 is a plot of the principal component loadings around the 1138-nm absorption band for CPM. The loadings appear spectra-like and are not noisy, indicating good modeling attributes for the factors chosen. The loading indicate regions of high correlated variance throughout the spectrum for each factor. Figure 7 is a plot of the PRESS. The model chosen used only six of these factors, trading decreased error for robustness (4). The PRESS for six factors was 0.0012. The resulting model had a multiple correlation coefficient (R2) value of 0.9987 and a standard error of calibration (SEC) of 0.0037 mg. The one-left-out cross validation demonstrates good predictability with a standard error of cross validation of 0.004 mg (very close to the SEC).
Figure 9
Figure 8 shows the NIR predicted CPM concentrations versus the HPLC results for each tablet in the calibration set using the synthetic calibration equation CPMsyncal2. The other five tablets scanned (tablet 6a through tablet 10a) on the MasterLab instrument with nominal levels of 1.0 mg CPM, that were not in the calibration set, were predicted for validation. Figure 9 shows the NIR predictions of the validation set versus the Lab (HPLC) CPM value. Table II shows the predicted values for the validation set. The standard error of prediction (SEP) of the validation set compared with the HPLC data was 0.0104 mg and the bias was 0.0139 mg. The SEP is significantly larger then the SEC because the synthetic calibration samples have reduced error except for the "seed" samples. The SEP is low at only about 1% of batch label claim.
Table II: Predicted values for the validation set with nominal value of 1.0 mg.
Conclusion
The authors demonstrated a method for generating a prediction model from placebo and "seed" batch samples from the production line with synthetic samples generated from average placebo and batch samples to increase the sample range. A prediction model with an R2 value of 0.9987 and a standard error of calibration (SEC) value of 0.0037 mg was developed. The standard error of prediction (SEP) on the validation set was only 1% of label claim at 0.0104 mg.
Acknowledgment
Thanks to Om Anand, Maria Gerald Rajan, Namrata R. Trivedi, Wen Qu, Yingxu Peng, and Yichun Sun who were at the University of Tennessee, Department of Pharmaceutical Sciences, at the time the CPM tablets were made and analyzed with HPLC.
Robert Mattes* is an applications scientist and Denise Root is a product manager, both at FOSS NIRSystems,
*To whom all correspondence should be addressed.
Submitted: July 14, 2008. Accepted: Aug. 12, 2008.
What would you do differently? Submit your comments about this paper in the space below.
References
1. FDA, Guidance for Industry: PAT-A Framework for Innovative Pharmaceutical Development, Manufacturing, and Quality Assurance (September, 2004, Rockville, MD).
2. R.A. Mattes et al., "Near-Infrared Assay and Content Uniformity of Tablets," Pharm. Technol. 31 (4), 170–182 2007.
3. R. Kramer, Chemometric Techniques for Quantitative Analysis (Marcel Dekker, Inc. 1998).
4. K.R. Beebe, R.J. Pell, and M.B. Seasholtz, Chemometrics: A Practical Guide (John Wiley & Sons, 1998).
Articles in this issue
almost 16 years ago
Pharmaceutical Technology, March 2010 Issue (PDF)almost 17 years ago
New Leadership and More Resources Aim to Modernize FDA Operationsalmost 17 years ago
Coming Down the Pike: Treating Epilepsyalmost 17 years ago
Inside USP: Heparin Monographs Further Revisedalmost 17 years ago
Changes to Vial Labels May Affect Patient Safetyalmost 17 years ago
A Call for Transparency in Research and Marketingalmost 17 years ago
Critical Challenges Require Core Valuesalmost 17 years ago
Detective WorkNewsletter
Get the essential updates shaping the future of pharma manufacturing and compliance—subscribe today to Pharmaceutical Technology and never miss a breakthrough.